Solving the most common pitfalls of tDCS therapies

Transcranial Direct Current Stimulation (tDCS) is a proven neuromodulation method whose effectiveness to treat neuropathic diseases such as Major Depressive Disorder (MDD) and chronic pain, among others, has been proven with a strong level of scientific evidence .
Using tDCS helps hospitals and clinics around the world to solve saturation and long queues in other neuromodulation services and offers patients who do not wish to take medication (or who cannot take it) an alternative treatment solution. However, tDCS therapies present their own shortcomings, and, although there are many tDCS therapeutic options in the market, not all devices are the same.
In this article, we see what the most common pitfalls of tDCS therapies are and how those can be solved:
Reproductivity of the treatment sessions and control of the stimulation area
Several studies suggest that the more accurate the reproductivity of the stimulation session (electrode placement, intensity of the current, duration), the better the treatment results are. Therefore, achieving an optimal reproducibility of the treatment session should be facilitated by any tDCS device meant for self-administration at home.
One of the main ways of achieving a good reproductivity of the electrode placement is by providing an easy-to-use cap, where the placement of the electrodes is pre-determined beforehand. Furthermore, offering different cap sizes adapted to the different circumferences of the cranium will ensure the best fit of the cap and a more snuggled positioning of the electrodes against the scalp. The use of other methods of placement of the electrodes on the skull such as bands, etc. is risky since they are more difficult to get into a 3-dimensionally accurate position.
When it comes to controlling the stimulation area, the optimization of the contact between the electrode and the skin is crucial. A good contact must be ensured by the addition of saline solution to a hydrophilic material to minimize discomfort when the electric current is transmitted to the scalp. However, the excess of saline can produce leaks that will cause a more diffuse stimulation area and, therefore, a less precise treatment administration.
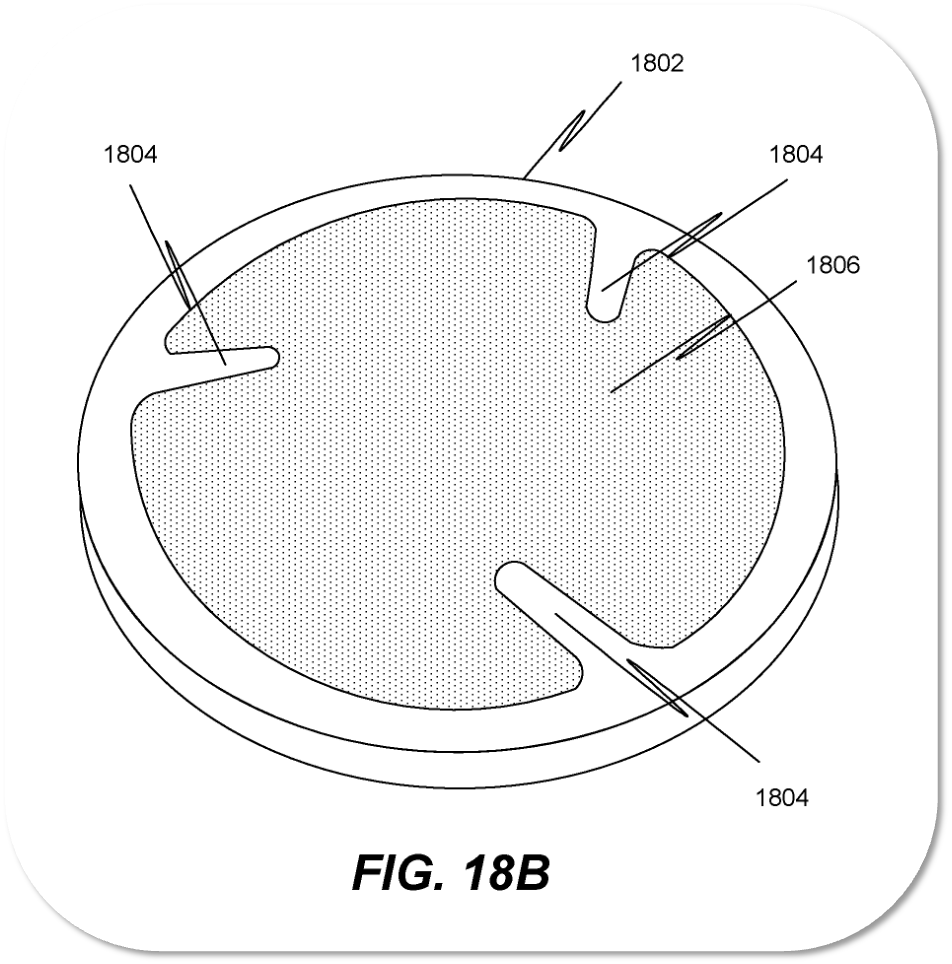
Cup-shaped electrodes can help to contain the saline solution within, avoiding unwanted spills furthermore, advanced technological materials such as Sooma’s proprietary electrodes and Hydrogel ensure a better contact with the skin and avoid liquid overflow contrary to what happens with traditional sponges.
Burns on the skin
Contrary to transcranial magnetic stimulation (TMS) therapies, where the application of a magnetic field is the means to obtain modulation of the neuronal activity, tDCS therapies are based on the application of a mild electrical current to the scalp. This method is generally safe and has only very limited side effects (redness of the area, itching sensation, and transient headaches). However, the uncontrolled application of electrical currents to the scalp, even if mild, may cause burns in the skin. To avoid this, it is important to ensure that the skin under the electrodes is not broken and that there are no metallic implants on the scalp that might warm up and cause burns. Furthermore, it is essential to measure the impedance of the area during the whole period of stimulation.
Impedance is a measure of the opposition to electrical flow and could be described as the “resistance” of the skin against the passage of electricity. When the impedance is high, the intensity of the electrical current needs to be augmented to obtain the same stimulation output to reach the brain, which can cause overheating and, ultimately, burns on the patient.
By constantly monitoring the impedance during the treatment duration and stopping the therapy if the impedance is too high, we can assure that the risk of burns is reduced. Also, the use of advanced technological materials such as Sooma’s proprietary electrodes and Hydrogel which ensure a better contact with the skin can significantly reduce the likelihood of burns on the scalp.
Informed consent of the patient
Most of the tDCS devices currently available in the market are only usable for research purposes. Since 26.5.2021, every brain stimulation device must be compliant with the Medical Device Regulation in the European Union, unless they claim legacy device status based on the old Medical Device Directive (MDR).
Compliance with the newest European Medical Device Regulation (MDR) is a challenge faced by many companies. Previously, a device could fall into medical device regulation depending on which kind of uses and applications their creators claimed. Taking advantage of that, some tDCS manufacturers did not claim any therapeutic benefits or applications for their products so they could launch them to the market without any kind of control.
However, the MDR regulation establishes that “equipment intended for brain stimulation that applies electrical currents or magnetic or electromagnetic fields that penetrate the cranium to modify neuronal activity in the brain”. In practice, this means that all brain stimulation devices must comply with the medical device regulation and that every device must have a clear indication of use for which it can be used. The manufacturer is thus required to provide a declaration of conformity document, which outlines the indication of use.
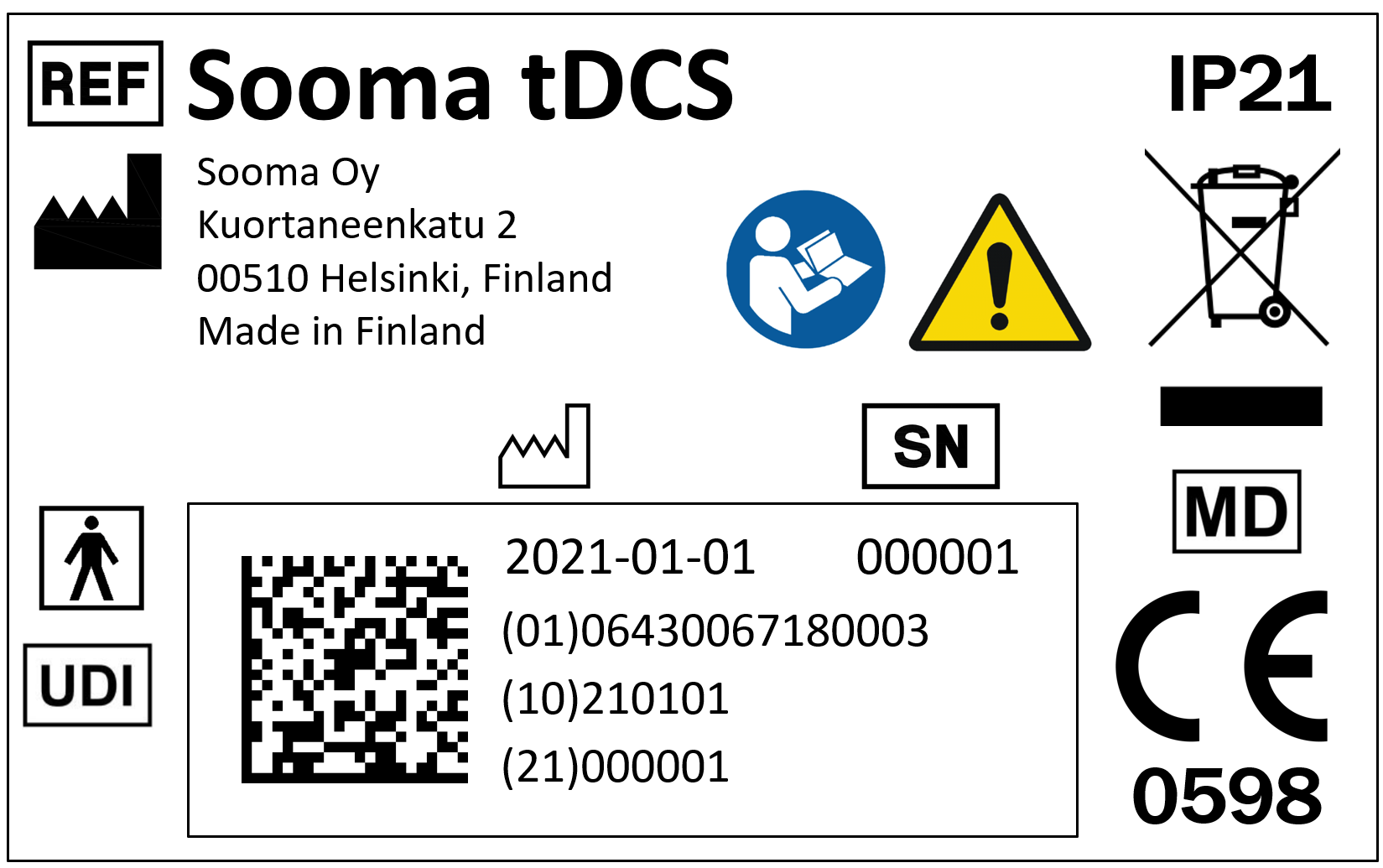
Furthermore, all brain stimulation devices belong to risk classification II or III, which means that their CE-mark should be followed by a four-digit number. This indicates the notified body, who is responsible for oversight of the manufacturer.
If the device does not have those four digits after the CE-mark or the manufacturer does not provide a declaration of conformity upon request, the device cannot be used for brain stimulation without an ethics committee approval, a clinical study plan, and informed consent by the patient.
Prescription of the therapy protocol and medical follow-up
Neuromodulation is a medical procedure that affects a vital organ such as the brain, therefore, the treatment prescribed by a professional and the possibility of following up the patient’s compliance when the therapy is administered at home is vital. Depression is a disease, where your condition may always worsen without adequate treatment and which can be life-threatening. It is imperative that a qualified clinician makes the decision about a patient’s treatment and follows them up appropriately. The largest risk, by far, associated with tDCS treatments for depression, is that more correct treatment is delayed, because of a previous incorrect treatment selection.
Prior to the administration of the therapy, it is necessary to have a medical diagnosis of the condition to be treated, as well as an established treatment protocol. Self-diagnosis of neuropathic disorders and unsupervised therapies can cause more harm than good to the patient in the long run. That is why tDCS devices should be only available to the patient via their healthcare professionals.
During the treatment protocol, it is important to ensure that the duration of the sessions and the intensity of the stimulation remains constant. For that purpose, having a device with fixed stimulation parameters is a great advantage, particularly in those cases where the patient is self-administering the treatment at home. However, a device with only one stimulation mode is quite limiting for the medical professional. That is why devices that can support several stimulation modes to be stored in their memory, in a manner such that only the clinician has access to them, is a great benefit.
Finally, being able to follow up on protocol compliance is an essential and sometimes overlooked feature. A device that shows the completed number of protocols, the use of disposable materials for the treatment administration, and the existence of remote monitoring tools for healthcare professionals such as websites are some of the ways in which the clinicians can monitor the progress of the therapy even when it is not being performed at the hospital or clinic.

TDCS is the treatment method offered by Sooma for depression (Sooma Depression Therapy, indicated for Major Depressive Disorder) and chronic pain (Sooma Pain Therapy, indicated for Fibromyalgia and chronic neuropathic pain). By using Sooma devices, you ensure that you are performing a safe and effective patient treatment, should be it in the hospital or at patients’ home, with legal, regulated, tested, and effective equipment that complies with the latest EU regulations and features all the recommended elements listed on this article.
Latest news

TGA approves Sooma’s at-home brain stimulation for depression in Australia
Read more
Sooma Medical Announces Pivotal FDA IDE Clinical Trial for At-Home Brain Stimulation Device for Depression Treatment
Read more
Sooma Pioneers the Integration of Brain Stimulation into Primary Care, Improving Access to Early-Stage Depression Treatment
Read more