Treating depression shouldn’t be hard

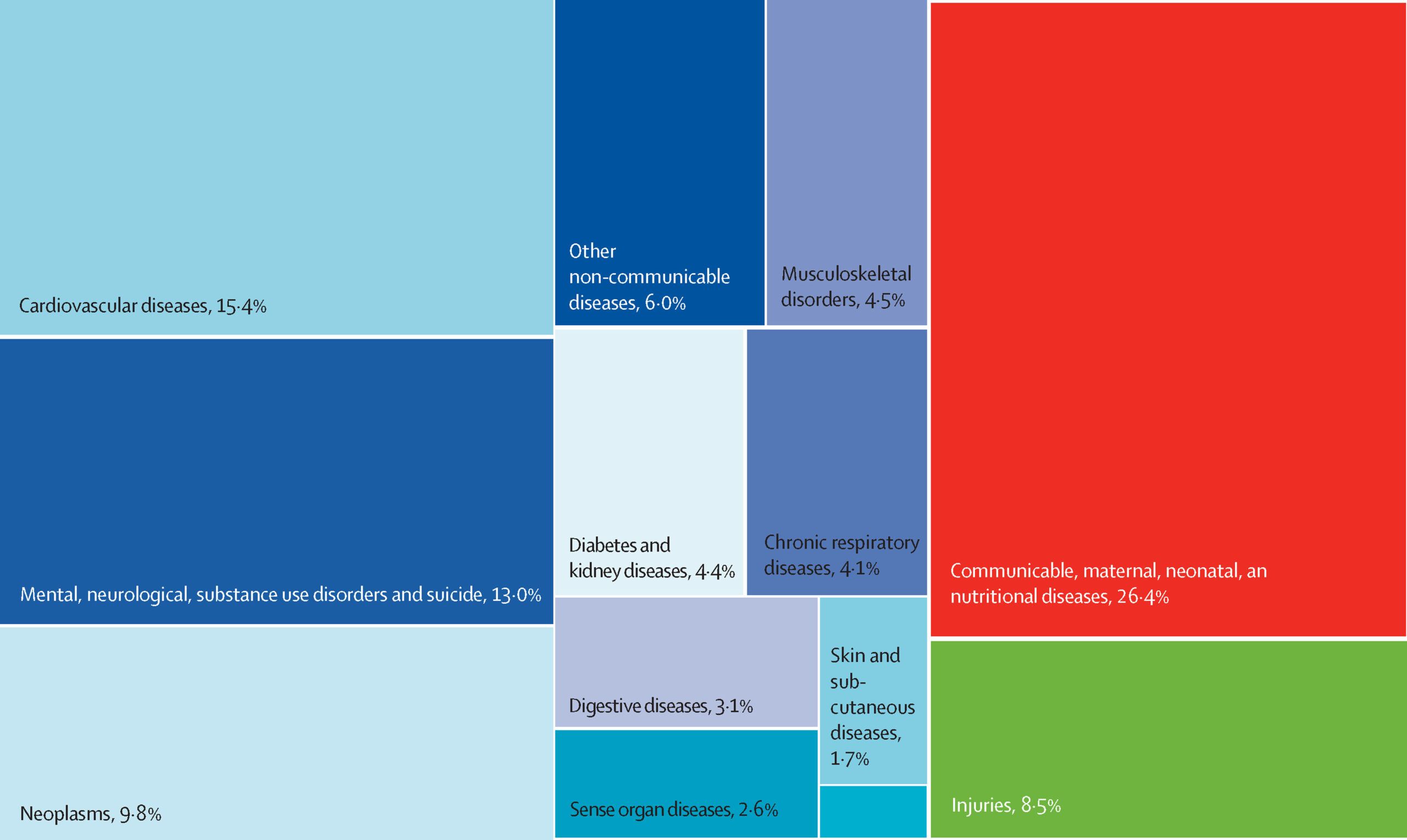
According to the World Health Organization, 1 billion people are estimated to suffer from a mental disorder1. Furthermore, 5% of adults (or around 280 million people) are estimated to live with depression, which makes this disease a leading cause of disability worldwide, and a great contributor to the global burden of disease. Despite these alarming figures, on average less than 2% of the countries’ health budgets are devoted to mental health matters. What are the reasons behind this lack of resources to treat depression when it is a widespread problem? Furthermore, what can be done to tackle this mismatch?
What are the factors that make treating depression challenging?
The term depression is used in health care to signify a condition influenced by several diverse factors which manifest in different ways and induce different outcomes. Depression is considered an “illness of the mind” diagnosed by the presence of at least five symptoms from a list of ten, among which either a “depressed mood” or a “markedly diminished interest or pleasure in activities” must be reported.
However, every episode of depression is unique, and therefore every patient experiences the episode differently, from its clinical presentation to its trajectory and rate of response to the treatment. Taken to the extreme, the complex nature of depression can lead to two individuals being diagnosed with depression without having any symptoms in common.
Other factors making the treatment of depression challenging are:
1 Depression is common but poorly recognised and understood
As seen in the introduction of this post, depression is a fairly common health condition, clearly different from the sadness that most people experience from time to time. Depression causes profound suffering to patients (and their relatives), impairs them to perform social and economic tasks appropriately, and elevates the risk of premature death by suicide or associated illnesses. And yet, these profound implications seem to be neither understood nor acknowledged, seen the insufficient funds devoted to mental health matters globally.
2 Depression is heterogeneous
The term depression often encompasses major depressive disorders, clusters of symptoms that lead to distress or social malfunction, as well as depression as experienced by people diagnosed with bipolar disorder.
Depression has a diversity of clinical manifestations, severity levels, and courses that often go beyond the boundaries set by current classifications, models and scores. Furthermore, there is still some uncertainty about what elements influence depression prevention and recovery and why they affect one individual and not another.
Therefore, more research is needed to develop and implement better treatment procedures and preventive strategies.
3 Depression is culture and context-dependent
The core features of depression have been described across human groups and populations since the very beginning of written clinical records. Sleep disturbances, depressed mood, or loss of interest and enjoyment are common manifestations of the disorder. However, depressive symptoms have significant variability of manifestations and prevalence, especially when considering the contextual, cultural cues and expectations of normal behaviour. Furthermore, the stigma associated with mental health issues in certain cultures might force depressed patients to disregard their condition for fear of being ostracised or subjected to mistreatment.
4 Depression and recovery are experienced differently by each patient
Depression is a multidimensional illness caused by a combination of factors: biological, sociological, and psychological, together with their interaction with proximal adversities. Furthermore, depression is associated with the patient’s overall physical health, and other ailments can develop a depressive episode. Each patient has a unique background and, therefore, a unique experience of depression. That, in turn, implies that they have special needs in terms of help, support, and treatment in recovery.
5 Depression treatment is difficulted by the care access gap
Current structural inequalities, particularly in countries where universal health care or mental health insurance are not present, mean that a considerable percentage of depression patients cannot obtain adequate treatment. Gaps in health care access make getting help almost impossible, especially over the longer term and for those patients with lower incomes.
6 Depression treatment needs a personalised approach
As we have established initially, every episode of depression is unique, and every patient experiences the episode differently. Therefore, a personalised clinical evaluation should be performed after diagnosing a depressed patient to assess their symptoms, personal values, preferences, and circumstances. This assessment will then ensure the correct personalisation of the treatment. However, the complexity of such a process is often limited in the context of limited care access and resource availability.
What can we do to offer a better response to depression?
Reducing the societal burden caused by depression is only possible with health policies based firstly on prevention and early detection. Then, there is a need for individual-level interventions that consider the patient’s environment, current life habits, and risk factors.
Mental health must have a pivotal role in universal health coverage, and its policies and impact must be handled beyond the health sector alone. Healthcare professionals, politicians, and researchers must make mental health care an integral part of their agendas, with a person-centred perspective that considers patients and their relatives when designing care plans, official policies, and novelty research.
Closing the inequality gap in healthcare access must be supported by a patient-centred approach, where treatment plans are tailored to the personal needs of the person suffering from depression, their relatives or caregivers, and their healthcare providers. In this sense, offering a wide range of treatment options will facilitate finding the most suitable choice for each individual. Offering home-based treatments, such as portable, easy to use tDCS devices like Sooma Depression Therapy, can also make access to treatment more straightforward and more flexible.
Creating more scientific and educational resources can help reduce the stigma associated with depression and better understand its heterogeneous and multidimensional nature.
To summarise, treating depression shouldn’t be hard. It is indeed a complex and multidimensional illness. Still, it can be effectively addressed by allocating the necessary resources and focusing on the emotional wellbeing of the patients with personalised treatments, inclusive policies, and care access.
TDCS is the treatment method offered by Sooma for depression (Sooma Depression Therapy, indicated for Major Depressive Disorder) and chronic pain (Sooma Pain Therapy, indicated for Fibromyalgia and chronic neuropathic pain). By using Sooma devices, you ensure that you are performing a safe and effective patient treatment, should be it in the hospital or at patients’ home, with legal, regulated, tested, and effective equipment that complies with the latest EU regulations and features all the recommended elements listed on this article.
- The Lancet (2022). Ensuring care for people with depression. 399, 10328, pp. 885.
Latest news

Sooma Announces Medical Technology Expert Andreas Hartlep as New CEO
Read more
TGA approves Sooma’s at-home brain stimulation for depression in Australia
Read more
Sooma Medical Announces Pivotal FDA IDE Clinical Trial for At-Home Brain Stimulation Device for Depression Treatment
Read more