Time to take action on mental health issues

There is plenty of evidence accumulated over the years that mental health issues are a major cause of avoidable suffering worldwide. Already before 2020, these issues were the main contributors to the global health-related burden, with depression and anxiety being the main influencing factors. With the emergence of COVID, the situation has deteriorated even further, as the pandemic has created a generalized environment where many triggers of poor mental health are present: deep-rooted structural inequalities, social isolation, bereavement, sickness, uncertainty, impoverishment, and poor access to health care.
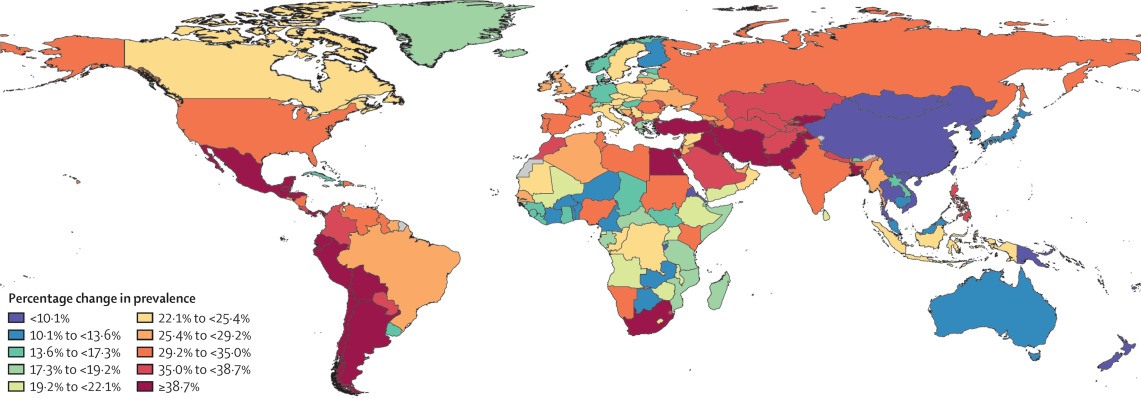
Thus, according to a recent scientific brief released by the World Health Organization (WHO), the global prevalence of depression and anxiety disorders increased by 25% during the first year of the pandemic with young people and women being the most affected collectives.
However, despite 90% of the countries which participated in the WHO research reported to have included mental health and psychosocial support in their COVID-19 response plans1, the figures above show that there has not been a huge success in preventing and alleviating these diseases.
Why are depression rates rising so much?
Although depression is a common health condition, on average, countries spend less than 2% of their health budgets on mental health matters2. There are several reasons why depression has not historically gotten the amount of attention and resources that it merits has one of the leading contributors to the global burden of disease.
The first reason has deep historical roots in the stigma that has accompanied mental health conditions in general, and depression in particular. Until the 20th century, the biological and physiological causes of depression were poorly understood, and the treatments used to cure patients weren’t always backed with strong scientific evidence. This stigma somehow continues still today, especially in underdeveloped countries, where inhumane treatments and forced institutionalization continue to be practiced despite the scientific advances that provide more effective treatments and the more widespread knowledge about the causes of depression.
Secondly, depression is a very heterogeneous illness whose management is not always straightforward. Patients, relatives, and clinicians alike are exposed to a wide range of symptoms, signs, severities, and evolutions of the illness, which make diagnosis and treatment challenging. This heterogeneity is also reflected in the patient response to the treatment, which can vary significantly, making it essential to offer new treatment options such as tDCS, for patients who do not obtain an adequate response from the first line of treatment.
In third place, depression is a multidimensional illness caused by a combination of factors: biological, sociological, and psychological. Therefore, it requires a multidimensional approach involving coordinated policies and investments across different public entities: healthcare services, education institutions, and social services.
Finally, the fourth reason lies in the existing structural inequalities, particularly in countries where universal health coverage or mental health insurance are not present. Gaps in health care access make getting help for depression almost impossible, especially over the longer term and for those patients with lower mean income.
How can we take action against depression?
For improving the prevalence rates of depression among the population, it is essential to create more scientific and educational resources and close the care access gaps.
Creating more scientific and educational resources can help reduce the stigma associated with depression and gain a better understanding of its heterogeneous and multidimensional nature. An integrated public health perspective towards depression must address its structural causes as well as the gravity, width, and duration of its consequences.
Closing the inequality gap in healthcare access must be supported by a patient-centered approach, where treatment plans are tailored to the personal needs of the person suffering from depression, their relatives or caregivers, and their healthcare providers. In this sense, offering a wide range of treatment options will facilitate finding the most adequate option for each individual. Offering home-based treatments, such as portable, easy-to-use tDCS devices like Sooma Depression Therapy, can also make access to treatment easier and more flexible.
In sum, the increment of adverse socio-economical factors caused by the COVID-19 pandemic has generated a so-called perfect storm which has, in turn, caused a major increase in the prevalence of depression and anxiety worldwide. These unexpected consequences of the pandemic have further underlined the urgency of making the prevention, early detection and diagnosis, and treatment of depression a generalized priority, which depends not only on supportive and non-stigmatizing societal networks but also on universal access to health care, and safe and efficient treatment options.
TDCS is the treatment method offered by Sooma for depression (Sooma Depression Therapy, indicated for Major Depressive Disorder) and chronic pain (Sooma Pain Therapy, indicated for Fibromyalgia and chronic neuropathic pain). By using Sooma devices, you ensure that you are performing a safe and effective patient treatment, should be it in the hospital or at patients’ home, with legal, regulated, tested, and effective equipment that complies with the latest EU regulations and features all the recommended elements listed on this article.
- World Health Organization (2 March 2022) COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide.
- The Lancet (2022). Ensuring care for people with depression. 399, 10328, pp. 885.
Latest news

TGA approves Sooma’s at-home brain stimulation for depression in Australia
Read more
Sooma Medical Announces Pivotal FDA IDE Clinical Trial for At-Home Brain Stimulation Device for Depression Treatment
Read more
Sooma Pioneers the Integration of Brain Stimulation into Primary Care, Improving Access to Early-Stage Depression Treatment
Read more